Early in its existence, Covid-19 gained an ability that would prove decisive in its relationship with human beings. The virus picked up a seemingly small change in its genetic code. It was likely an unfortunate accident – a fragment of genetic information from another virus got muddled up with that of the coronavirus while they were both infecting a bat.
Included within this tiny piece of genome, however, were the instructions that altered a key part of the virus – its spike protein. This important protein studs the outside of the coronavirus and is the part that attaches to the outside of cells, helping the rest of the virus to sneak inside where it can replicate.
This change to Covid-19's spike protein meant it could hijack an enzyme found in the human body called furin. This enzyme acts like a pair of molecular scissors, normally cutting open hormones and growth factors to activate them. But when furin snips part of the Covid-19 spike protein, which is normally folded in a series of loops on the outside of the virus, it opens like a hinge.
"This exposes a new sequence in the spike protein," says Yohei Yamauchi, a reader in viral cell biology at the University of Bristol, UK, who has been studying how this change may have led Covid-19 to become more infective in humans. "It is one of the changes that make this virus really different from previous coronaviruses that caused Sars and Mers."
This new mutation meant Covid-19 could suddenly latch onto an important molecule found scattered around the outside of human respiratory cells called Neuropilin 1. This molecule helps to transport material inside cells and deeper into tissues – the mutation was like handing Covid-19 the keys to a new door into our cells and meant the virus could replicate in greater numbers in the human airways.
Although this mutation was just one in Covid-19's short existence, it proved to be important. Some researchers believe it may be one of the key mutations that allowed the coronavirus to jump species and begin causing a rapidly spreading disease in humans. But almost as soon as it did this, it began picking up other mutations.

Scientists have been able to track how the virus is evolving in swab samples taken in Covid-19 testing centres (Credit: Prakash Mathema/Getty Images)
With almost every person it infects, the virus changes very subtly – picking up a letter in its genetic code here, another being deleted there or swapped for something different. Most have little effect other than helping scientists to trace how the virus is spreading around the world. But occasionally a mutation occurs that alters how quickly the virus spreads, how infectious it might be or even the severity of the disease it causes.
Understanding what might be driving some of the changes to the virus and what they do to its behaviour could prove essential as the pandemic continues. Here are some of the most important changes that Covid-19 has undergone so far.
The super shedder
The mutation that allowed furin to cut the spike protein was already present in the Covid-19 virus as it began to infect people in Wuhan in early December. A few short months later, the first cases began to be detected in Europe and a major change in the virus occurred that would prove significant for the course of the pandemic.
Although there is now evidence to suggest Covid-19 had arrived in Europe as early as December 2019, the virus was initially spotted spreading in northern Italy in February 2020.
Samples taken from there on 20 February revealed the virus had undergone a mutation on the spike protein that dramatically increased the number of viral particles that were shed by infected cells, particularly in the upper respiratory tract of patients.
Recent analysis, however, suggests this variant may also have originated in China and had been circulating in a number of provinces there in late January 2020. It was even found to have made its way to Bavaria, Germany, on 28 January 2020 via someone travelling from Shanghai, suggesting it was introduced to Europe on a number of occasions from China.
The mutation the virus picked up is known as D614G, and this change seems to have enabled the virus to spread more quickly between people, probably because infected people coughed and breathed more of the virus out.
D614G gives the Covid-19 spike protein a more "open" structure, which improves its ability to bind to another receptor found on the surface of human cells called ACE2. Covid-19's ability to bind to ACE2 was already known to be one of the reasons it had been able to start infecting humans in the first place, but this new mutation gave it an increased ability to target human cells.
You might also be interested in:
- How Covid-19 might mutate in the future
- The other coronavirus worrying experts
- How effective is a single vaccine dose
Subsequent research has suggested that D614G made the virus more infectious than the original version that emerged from Wuhan and appears to have been more common in younger people. But this also came at a cost – the mutation may have also left the virus more vulnerable to antibodies, meaning it was less able to cause reinfections in people who had already had the disease. This also meant it could be combated using convalescent plasma from patients who had already recovered.
Despite this, the D614G variant quickly became the dominant form of the virus around the world.
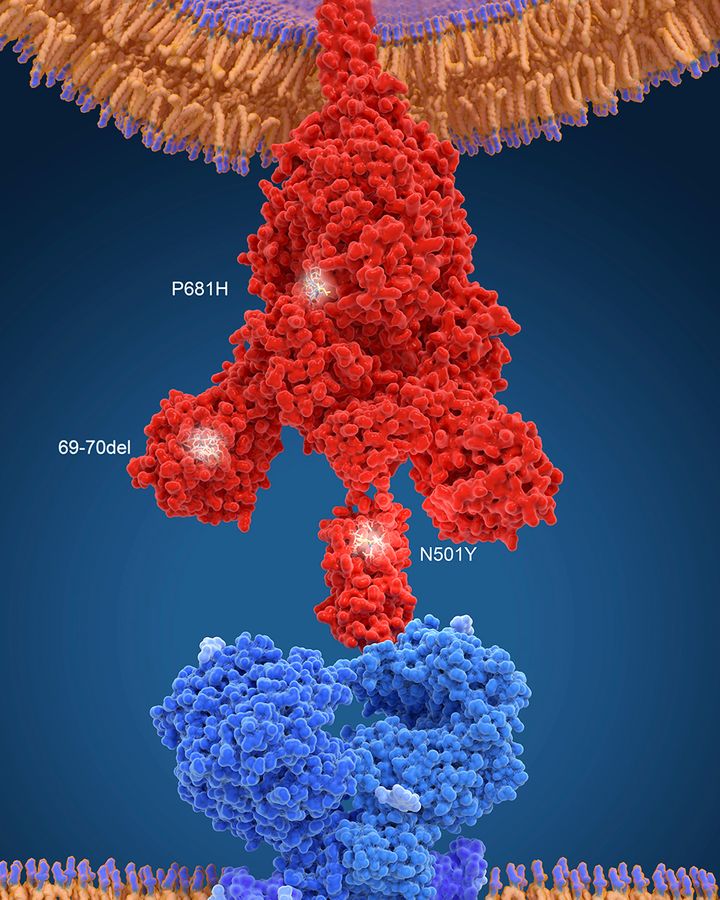
The new British variant of Covid-19 has several mutations on the spike protein that allows the virus to bind to human cells (Credit: Science Photo Library/Getty Images)
The holiday virus
Then, as lockdowns eased in Europe over the summer and international travel began to rise again, another significant new variant of Covid-19 emerged in Spain. First detected in June 2020, it spread throughout Europe and by September it accounted for 50-70% of cases in Switzerland, Ireland and the UK.
Named 20A.EU1, or more commonly the "Spanish variant", this version of Covid-19 picked up a mutation on its spike protein that was designated A222V. But the mutation does not occur in an area that binds to the cell surface, so is unlikely to have produced increased infectivity. Instead, researchers believe its rapid spread and high prevalence is more incidental – due to the spurt of travel that occurred over the summer as people squeezed in a holiday while restrictions were eased.
The antibody evader
While A222V mutations don't appear to have led to a dramatic change in the virus's behaviour, another mutation that emerged in Scotland during March 2020 set some alarm bells ringing. This mutation – known as N439K – was discovered in around 500 samples taken from patients in Scotland but by June appears to have died out in the country, possibly due to the reduced spread thanks to strict lockdown restrictions.
The mutation to the Covid-19 spike protein not only appears to have increased its ability to bind to ACE2 on human cells but variants carrying this mutation have also shown some resistance to antibodies taken from patients who have recovered from the virus. It has raised concerns about the virus's ability to cause reinfections. But experts say that it does not appear to cause any increase in severity of the disease in patients. A recent report by the Covid-19 Genomics UK Consortium (Cog UK) adds "there is no evidence that this mutation will allow the virus to impair the immunity triggered by vaccines".
In the autumn, however, new occurrences of this mutation in Covid-19 appeared – apparently independent of those seen in Scotland – elsewhere in Europe and also in the US where they continue to spread. It is also now occurring alongside another mutation – the deletion of two apparently key amino acids on the spike protein, H69 and V70.
The repeat offender
In fact, the H69/V70 deletion has been popping up all over the world. Scientists first began seeing it in samples in Thailand in January 2020 and then in Germany the following month, although both appear to have occurred independently.
The H69/V70 deletion has been found to produce a change in the shape of the Covid-19 spike protein so that a loop of molecules that normally protrude from it are pulled in tighter. Although it is not totally clear what benefit this might give the virus, it has been suggested it may be an adaptation by the virus as it tries to evade the immune system, although no change in the severity of the disease or impact on vaccines has been spotted.
Ravinda Gupta, a clinical microbiologist at the University of Cambridge who was among the first to identify the B117 variant, says the H69/V70 deletion mutation "increases the infectivity by twofold".

Millions of mink have been culled in Denmark after a variant of Covid-19 was found to be passing from the animals to humans (Credit: Mads Claus Rasmussen/Getty Images)
An analysis of virus sequencing data from around the world suggests H69/V70 deletions have occurred multiple times in Covid-19. For much of last year it spread quietly, then a cluster of patients infected with the virus carrying a H69/V70 deletion appeared in Denmark. This mutation was appearing in a version of the virus that was being passed from mink on farms to humans. While analysis showed the virus had mutated slightly to become more infectious to the animals, some early data suggested it was also less sensitive to antibodies contained in the blood serum of patients who had recovered from Covid-19.
In August, however, the H69/V70 deletion started to become far more common and was appearing in virus samples alongside the N439K mutation.
The British variant
This same H69/V70 deletion is one of the main features in the rapidly spreading B117 "British" variant of Covid-19. Alongside this change, B117 has accumulated 16 other mutations on its spike protein. "Many of the mutations that are seen in this new variant are ones that we haven't really seen before," says Gupta.
Among those is a mutation neighbouring the furin cleavage site on the spike protein that proved so important in Covid-19's ability to become a pandemic strain in the first place. This mutation, known as P681H, has been found in other variants around the world before, including in a lineage of the virus that emerged in Nigeria in December, called B11207.
The difference with the British variant is that it carries another important mutation known as N501Y, which occurs in a key region the virus uses to bind to cells. It is thought to help the virus bind more tightly to the ACE2 receptor on the outside of cells.
Although the exact impact of the other individual mutations that have occurred in the British variant are still to be fully explored, when combined, they have led the virus to become more transmissible between people. This is perhaps because those infected with the virus produce more infectious particles than with previous variants. It mean more of the virus is expelled in tiny droplets by infected individuals when they cough, talk and breathe.
Scientists have estimated that B117 replicates itself twice as fast as the strain that emerged from Wuhan. Some public health officials are now predicting that B117 will become the dominant form of Covid-19 in many countries, including the US.
Exactly how the British variant occurred is still not clear, although it is not thought to have accumulated so many mutations gradually. Their sudden appearance together is a clue for some researchers.
"The working hypothesis is that this happened in a chronically infected individual," says Gupta. There have been at least two cases of H69/V70 deletions occurring alongside other mutations in patients who have been chronically ill with Covid-19 – one in an elderly woman in Moscow, Russia, and the man in Cambridge, UK.
Both had received treatment for cancer which is thought to have reduced the ability of their immune systems to fight off Covid-19. Because the patients were infected for so long, the virus had time to replicate to high levels in their bodies and accumulate mutations. When the patients were given antibody therapy, those versions of the virus that were better able to escape or outpace the treatment survived.

News of the B117 variant spreading rapidly in England led many countries to close their borders temporarily, leading to long tailbacks (Credit: William Edwards/Getty Images)
"We don't know where this might have happened yet with B117, but in long-term infections the virus has a chance of fighting off a bit of genetic pressure from a treatment," adds Gupta.
Recent mortality data released in Britain seems to suggest that the B117 variant is up to 30% deadlier than the earlier versions of the virus, but this is yet to be confirmed in peer-reviewed scientific studies. Even so, Gupta doesn't believe B117 will pose a problem for the current vaccines being rolled out around the world. One recent study showed that antibodies produced by participants in the Pfizer vaccine trial do seem to act against this variant.
"But this is a warning sign that we need to not be complacent," says Gupta.
The South African Variant
Shortly after news of the B117 variant broke, scientists in South Africa revealed that they too had identified another mutated Covid-19 virus spreading within their own country.
"Following the first wave of SARS-CoV-2, we observed rapid resurgence of infections in two regions of South Africa – the Eastern and Western Cape Provinces," says Carolyn Williamson, head of the division of virology at the University of Cape Town. She and her colleagues intensified their sequencing of viruses from Nelson Mandela Bay and Garden Route district in these two areas and found that a new variant had emerged in mid-October and rapidly come to dominate in these two regions by the end of November. By December the variant – called 501Y.V2 or B1351 – had spread to a number of other areas of South Africa and was also detected in neighbouring Zambia. It has since been found in at least 20 other countries in travellers and has shown signs of spreading locally in some too.
A recent study has shown that the South African variant is able to escape antibodies in the blood plasma of patients who caught Covid-19 during the first wave of the pandemic. While this could be seen as a worrying sign that current Covid-19 vaccines may be less effective against this variant, it is important to remember that antibodies only form one part of the immune system's response to the virus. Other types of immunity, such as that provided by T cells, could still be effective, although this has still to be tested.
Williamson and her colleagues found that this version of the Covid-19 virus carries eight distinctive mutations in the spike protein, including three that are thought to have contributed to its higher transmissibility.
"We do not know how this variant emerged," says Williamson. But she speculates that it may have also occurred in someone with a long-lasting infection. "Usually SARS-CoV-2 is an acute infection and rapidly cleared... in some individuals there may be ongoing replication allowing for viral evolution to occur."
Among the mutations Williamson and her team detected was the N501Y mutation also seen in the British B117 variant. Another of the mutations – K417N – has been suggested to combine with N501Y to increase the strength with which the virus can bind to the ACE2 receptor on human cells, but other computer modelling work has suggested K417N may counteract the increased binding seen in N501Y.
There is currently no indication it causes more serious disease, but it seems to spread more rapidly than previous forms of the virus. "A virus that is more transmissible and less pathogenic is more likely to survive," says Williamson. This is because if a virus kills its host too quickly, it will not have time to replicate as much and spread to other people.

The new variant spreading around Brazil has shown signs that it can reinfect people who have already had the virus (Credit: Mauro Pimentel/Getty Images)
Studies have suggested, however, that the K417N mutation may reduce the virus's sensitivity to human antibodies. A third mutation called E484K – which is not present in the British variant – also seems to reduce the virus's vulnerability to antibodies. One study suggests that changes to the E484 site in the spike protein can produce a 10-fold reduction in the ability of some antibodies to neutralise it.
The Brazilian variant
The E484K mutation is proving to be important in another concerning variant that is now spreading around the world. The P1 variant contains 20 unique mutations, including the E484K change found in the South African variant. It seems to have first emerged in the city of Manaus, Amazonas state, in north Brazil, which has been particularly severely hit by the pandemic. The variant was also detected in four travellers who had flown from northern Brazil to Japan on 2 January this year.
This version of the virus also carries the N501Y mutation alongside the E484K change and one called K417T. Although the exact consequences of these mutations are still being investigated by scientists, the strain has been designated as a "Variant of Concern" by global health officials.
The emergence of the Brazilian P1 variant raises concerns that the virus may be developing an increased propensity for re-infecting individuals, according to the US's Centre for Disease Control and Prevention.
Another Brazilian variant, designated P2, has been found in two people who caught Covid-19 a couple of months apart. This variant, however, carries the E484K mutation, but lacks the other two that are concerning scientists about P1.
While the E484K mutations have raised concerns that the virus might be evolving in ways that allow it to evade parts of the immune system, scientists from the Cog-UK consortium have said there is no evidence yet to suggest that it is affecting the effectiveness of the vaccines.
But as Covid-19 continues to mutate, many virologists are looking at ways to help them get ahead of the virus. Michael Worobey, a viral evolutionary biologist at the University of Arizona, and his team are developing an "early warning" test that might help detect new potentially worrying variants of Covid-19 as they start spreading. (Read more about how Covid-19 might mutate in the future.)
"We already have good information from laboratory studies about which amino acid changes are likely to be the most worrisome," he says. "So, we can use this to hopefully catch them early." That should help public health officials and vaccine manufacturers be more prepared when the virus undergoes its next major change.
--
Join one million Future fans by liking us on Facebook, or follow us on Twitter or Instagram.
If you liked this story, sign up for the weekly bbc.com features newsletter, called "The Essential List". A handpicked selection of stories from BBC Future, Culture, Worklife, and Travel, delivered to your inbox every Friday.
"how" - Google News
January 28, 2021 at 10:16AM
https://ift.tt/3r3lQ6N
How Covid-19 mutations are changing the pandemic - BBC News
"how" - Google News
https://ift.tt/2MfXd3I
https://ift.tt/3d8uZUG
Bagikan Berita Ini














0 Response to "How Covid-19 mutations are changing the pandemic - BBC News"
Post a Comment